If you’re like most older adults, taking multiple medications is part of your daily life. Safe medication management is a critical part of living well with chronic illness. “Medications are important – we take them to treat disease and live longer,” says Susan Love, a nurse case manager at Amedisys Home Health in Harrogate, TN. “If we aren’t monitoring those medications and teaching patients how to take them appropriately, then we aren’t truly managing their disease.”
Why is Medication Management Important to Patient Safety?
As many as 83% of adults in their 60s and 70s take at least one medication, and one-third use five or more.1 The more medications you’re prescribed, the harder it is to take them properly. You also have a greater risk of negative reactions and interactions, called adverse drug events, which are responsible for at least 1.5 million emergency room visits and nearly 500,000 and hospitalizations each year. 2
It’s easy to become overwhelmed or confused by taking multiple medications, leading to mistakes. This can be even more difficult to manage if you are seeing multiple doctors or specialists and facing frequent hospitalizations.
Some common mistakes include:
- Taking too much or too little medication
- Missing doses
- Not stopping a medication that you were supposed to no longer take
- Stopping a medication without talking to your doctor
Sometimes, medications can cause problems even when they’re taken correctly, so it’s also important to recognize possible problems and report them to your healthcare provider right away. Some common medication-related issues include:
- Allergic reactions
- Drug interactions (when one medication affects how another one works)
- Drug-disease interactions (when a medication for one condition affects another one negatively)
- Food-drug interactions (when what a person eats or drinks affects how a medication works, potentially causing side effects or reducing its effectiveness)
- Side effects (which can range from unpleasant to dangerous)
Expert Medication Management Tips for Seniors
Let’s take a closer look at common medication management challenges for seniors and some tips that can help you overcome them.
Medication Challenge #1: I’m taking so many medications, it’s hard to keep track of how and when to take them
Taking medications correctly helps prevent avoidable hospitalizations and helps you manage your illness. If your medication routine is too complicated, ask your doctor or pharmacist to help you simplify the process.
You can help prevent medication errors with these simple tips:
- Make a list of your medications and keep it up to date. Check your list with your doctor or pharmacist at each visit.
- Only take your own medication. Do not take any medicine prescribed to someone else.
- Follow the directions on the label. Get in the habit of checking the label to verify the name of the medicine prescribed to you, the amount you are supposed to take and when you are supposed to take it.
- Do not double your dose if you miss a dose.
- Do not increase, decrease or stop taking your medications just because you feel better. Check with your doctor, pharmacist or nurse first.
- Do not take any additional medications or supplements, including over-the-counter medications like cough or allergy medicine, without calling your doctor, pharmacist or nurse first.
- Use a pillbox. This will prevent you from missing doses.
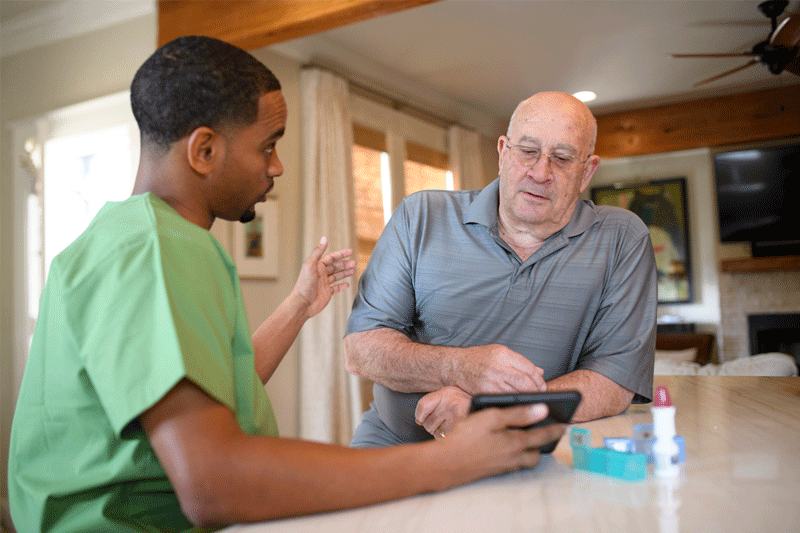
- Consider using a medication tracking app. There are many health/medication tracking apps that will send alerts and reminders for missed doses and help you organize a medication schedule.
- Ask your pharmacy if they offer individual packaging. Some pharmacies will provide monthly prescriptions in daily dose packaging, rather than pill bottles. (These are not child-safe, so consider your individual situation.)
- Keep all medications in one area and follow the instructions on the label on how to store the medication.
- Take medicines at the same time each day. Set an alarm or ask a friend or family member to remind you to take your medicine.
Medication Challenge #2: I don’t want to take another medication; do I really need this?
It’s possible you don’t need a medication because another medication you’re taking serves the same purpose. It’s also possible that you need the medication, but don’t fully understand why. “Medication management is largely about education,” says Love. “When you know what a medication is for and how it helps you, you’re more likely to take it as directed.”
You can figure out if you need a medicine by asking the following questions any time a doctor gives you a new prescription:
- Why do I need this medication? What does it do?
- How do I know if it’s working?
- What are the pros and cons of taking this medication?
- Is there anything I can do that may prevent me from having to take this medicine?
- How often should I take it? At what time?
- Are there things I shouldn’t do or eat/drink while taking this medicine?
- How long will this medicine take to work?
- Am I taking the lowest effective dose?
- Is it okay to take this medicine with the other medicines I’m taking?
- When should I stop taking this medicine? Will I be on this medication for the rest of my life?
- What should I do if I forget to take my medicine?
- What side effects should I look for? What should I do if there’s a problem?
- Will I need to refill this medicine when it runs out? How do I do that?
- How should this medication be stored?
At each appointment, ask if the medication is working, if you still need it and if you’re still taking the correct dose. Do not stop taking a medication without clearing it with your doctor first.
Medication Challenge #3: I just found out two of my medications interact with each other
Many older adults see several different doctors, who don’t know what the other is prescribing. To guard against harmful drug interactions, create a medicine log you can take with you to every doctor’s appointment and pharmacist visit. This helps them to do an accurate medication reconciliation, or update, to your medication record with them.
This medication log should be kept somewhere visible, like on the fridge, for your caregiver and family members to read. You should also always carry a copy with you so if an emergency happens, a first responder can see what you’re taking and care for you properly.
Your list should include:
- Every medicine you take (both generic and brand names), including prescription drugs, over-the-counter medications, dietary supplements and herbal remedies
- Reason for taking it
- Name of prescribing doctor
- How often you take it and at what dose
- How you take the medicine (by mouth, injection, under the tongue)
- Side effects
Visiting just one pharmacy can also cut the risk of drug interactions and double dosing on the same medication. “Find a good pharmacy that offers medication management support, like calling patients when a medication is due to be refilled,” Love recommends. “And use that pharmacy for all your prescriptions.” Be sure to tell your pharmacy if your doctor discontinues a medication so it doesn’t refill a medication that you no longer need.
Medication Challenge #4: There are too many side effects
Many people stop taking their medication because they don’t like how it makes them feel, but there are often ways to minimize side effects if you pay attention to them, write them down and report them back to your doctor.
You can also minimize side effects by taking medications as directed by your doctor. For example:
- Store them properly (some need a dark environment or to be refrigerated).
- Don’t drink alcohol or use illicit drugs (and if you do, tell your doctor so they can look for interactions).
- Don’t take medications prescribed for someone else (or share yours).
- Tell your doctor if you have any allergies.
- Take your medication with food or on an empty stomach, as directed.
- Talk to your doctor about an alternative medication if side effects are too bothersome or disruptive.
Medication Challenge #5: I can’t afford my medications
The cost of prescription drugs has forced many seniors to choose between medications and food. The AARP reports that 48% of adults over age 50 have skipped a medication due to cost or know someone who has. 3 If you’re skipping medications because they’re too expensive, consider:
- Asking your doctor if you can switch to a cheaper medication or if samples are available
- Asking your pharmacy for alternate ways to get your medications, including discount programs through the manufacturer
- Comparing prescription prices at pharmacies near you on smartphone apps like GoodRx, which also offers prescription discounts
“Doctors often aren’t aware how much prescriptions cost,” says Tara White, a licensed practical nurse at Amedisys Home Health in Toccoa, GA. “In many cases, there’s a cheaper medicine that’s just as effective if you ask.”
Most older adults want to stay home and out of the hospital. Taking medications as directed may help you do this. If you need more support with medication management, talk to your doctor. There are tools that can help, and you may be eligible for in-home nursing visits for medication administration and education, as well as occupational therapy and other services through a local home health care agency.
Carolyn Hartsfield, MBA, RN, serves as Assistant Vice President of Nursing Strategy Innovation Programs at Amedisys. With 30 years of nursing experience, including 28 years in the home health industry, Carolyn brings a wealth of expertise to the field. She is passionate about improving home health services and dedicated to making a lasting impact in the industry.