Hospice and palliative care are two different types of care that are often confused. Both provide pain and symptom relief for people with serious illness, but there are important differences. Learning more about the difference between hospice and palliative care will help you find the right care for your situation.
When comparing palliative care vs. hospice, it’s useful to know the definitions of each as a starting point.
What is Palliative Care?
The definition of palliative care is care that provides relief from symptoms of a serious illness and side effects of treatments. Palliative care is an option before there is a need for hospice. Patients can receive palliative care when they’re first diagnosed with a serious illness. They can also receive care while working toward a cure or transitioning to end-of-life care. With the support of palliative care, patients may be able to feel better, continue working and doing daily activities, and recover.
The Definition of Palliative Care: Important Facts
Here are some important facts about the definition of palliative care:
- The main goals of palliative care are helping patients feel better and improving their quality of life. [1]
- Palliative care is a consult-based program with nurse practitioners who help patients and families manage chronic illnesses such as cancer, dementia, amyotrophic lateral sclerosis (ALS), and kidney, heart and lung diseases. [2]
- Some of the services commonly offered in palliative care are pain and symptom management, goals of care discussions, advanced care planning, family meetings, education and support.
- Patients can transition from palliative care to hospice care as their disease progresses toward the end of life.
- Some of the professionals that may be on the palliative care team are doctors, nurses, dietitians, social workers and chaplains.
- Palliative care helps patients coordinate with their primary care physician, specialists, and community resources to get the right care and support for their complex and chronic health needs.
Hospice Definition
Hospice is defined as care for people diagnosed with a terminal illness who are expected to live months rather than years. It is sometimes called “end of life” care.
People often choose hospice care when treatment is no longer working, or they don’t want to continue curative treatments for a terminal disease. Hospice is for people who want to maximize the time they have left, surrounded by what matters most to them.
It’s important to know that hospice is provided wherever the patient calls home, whether that be their private residence, a family member’s home, a nursing home or other location.
Here are some important facts about the hospice definition:
- The focus of hospice care is comfort and quality of life.
- Hospice includes palliative care, plus added services.
- Some of the services commonly offered in hospice care are pain and symptom management, goals of care discussions, advanced care planning, family meetings, education and support.
- Hospice care may include regular visits from nurses, nurses’ aides, social workers, chaplains and trained volunteers.
- Medicare, Medicaid and most private insurance plans cover hospice costs for qualifying patients.
- As long as a physician certifies a person is eligible, hospice care can be extended if necessary. A person can also change their mind about hospice anytime.
- Family caregivers get a lot of support while their loved one is receiving hospice care. This may include education, respite care and bereavement support.
10 Ways Hospice and Palliative Care are the Same
It’s important to understand the difference between hospice and palliative care, but let’s start with the similarities. Both offer:
- Compassionate care for patients with serious illnesses
- Pain and symptom relief
- Greater independence and control
- Fewer unnecessary trips to the hospital
- Comfort and quality of life as the primary goals
- Physical, emotional and spiritual support
- Treatment teams made up of professionals with a variety of special skills
- Social and emotional support for family caregivers
- Education on health conditions and what to expect during care
- Care coordination with the patient’s current primary care doctor/healthcare team
8 Differences Between Hospice and Palliative Care
Understanding the differences between these two services can help you decide when to choose palliative care vs. hospice care. Let’s take a look at some of these key differences.
How is Palliative Care Different from Hospice?
1. Start Time
- Palliative care can start at any stage of an illness. This includes when the person is diagnosed, when they’re receiving treatment to cure their illness or when they’re nearing the end of their life.
- Hospice care begins in the later stages of illness, when the person is expected to live about six months and is also called end of life care.
2. Goals of Care
- When a patient chooses palliative care, quality of life and comfort is key. However, patients can receive palliative care at the same time that they’re trying to cure their illness. Their goal is to recover and/or extend life while staying as comfortable as possible.
- When a patient chooses hospice, the goals of care shifts from curing illness to focusing on comfort and quality of life.
3. Payment
- Palliative care costs are usually paid for by insurance or out of pocket by the patient. Some costs may be covered by Medicare, Medicaid or private insurance, depending on the patient’s plan.
- Hospice costs are 100% covered by Medicare, Medicaid, the Veterans Administration and most private insurance plans for qualifying patients.[3] Benefits cover the cost of hospice services and medications, as well as medical equipment and supplies related to the terminal illness. Medications and services that are unrelated to the terminal illness fall under the patient’s traditional Medicare, Medicaid or private insurance benefits.
4. Frequency
- Palliative care visits are dependent on each patient’s needs as they change. In some cases, this can be weekly, monthly or even less frequently.
- Hospice care involves regular visits from a nurse, certified nurses’ aide and other hospice staff including chaplains, volunteers and more. These visits may happen multiple times per week, depending on the patient’s needs.
5. Eligibility
- Since Medicare only covers parts of palliative care, patients do not need to meet specific requirements to be eligible.
- To receive hospice under Medicare, patients must meet eligibility requirements (prognosis of six months or less as determined by a doctor). [4]
6. Length of Care
- Palliative care is available starting upon diagnosis and continuing until the patient’s illness is cured or they transition to end-of-life care.
- Patients can receive hospice care for six months or longer if a doctor certifies that they continue to meet eligibility criteria. [5]
7. Location
- Palliative care can also be provided at home or in a hospital or facility. In some cases, palliative care is offered through special outpatient clinics, where patients may travel to visit with palliative care providers.
- Hospice is provided wherever the patient calls home, whether that be a private residence, a nursing home, a hospital or other location. Patients do not have to travel to receive these services.
8. Support
- Palliative care may include nursing visits but focuses heavily on advanced care planning and care coordination, helping patients to work with resources available to them to receive additional support in the home.
- Hospice services include in-home care, such as nursing care, a certified nurse’s assistant who can help with activities of daily living and other support.
Palliative Care and Hospice FAQs
By understanding the similarities and differences between palliative care and hospice, you may now have a better idea of which service would be most helpful for your situation. To help you learn a few more details, these FAQs may be useful:
1. What Symptoms Does Palliative Care Treat?
Common symptoms that palliative care may help with are pain, nausea, shortness of breath, fatigue, decreased appetite, constipation, anxiety, depression and difficulty sleeping.
2. Can I Keep My Doctor if I Choose Palliative Care or Hospice?
Choosing either palliative care or hospice does not mean your primary care doctor is no longer involved in your care. Both palliative care and hospice will work together with your primary care physician to plan the best treatment for your goals of care.
3. Can I Change My Mind About Palliative Care or Hospice?
Sometimes circumstances change after a patient has enrolled in palliative care or hospice. For example, a person who is receiving hospice care might decide to resume curative treatment. It is always ok to decide to stop receiving these services, and you can start palliative care or hospice again at a later date.
4. Do Palliative Care or Hospice Offer 24/7 In-Home Care?
Whether you’re a patient or a caregiver, you may wonder if round-the-clock care is a part of either palliative care or hospice. In both of these cases, home visits are intermittent. Hospice offers 24/7 on-call care for any sudden concerns or changes. Some palliative care programs do as well. Palliative care and hospice can both help families locate resources to help with ongoing care needs, and hospice can offer respite care (with limitations).
Although there are many differences between hospice and palliative care, both types of care can make a difficult time easier for patients and their families. If you’re struggling with a serious illness, ask your health care provider which is the best option for you, palliative vs. hospice. To learn more, call a care center near you.
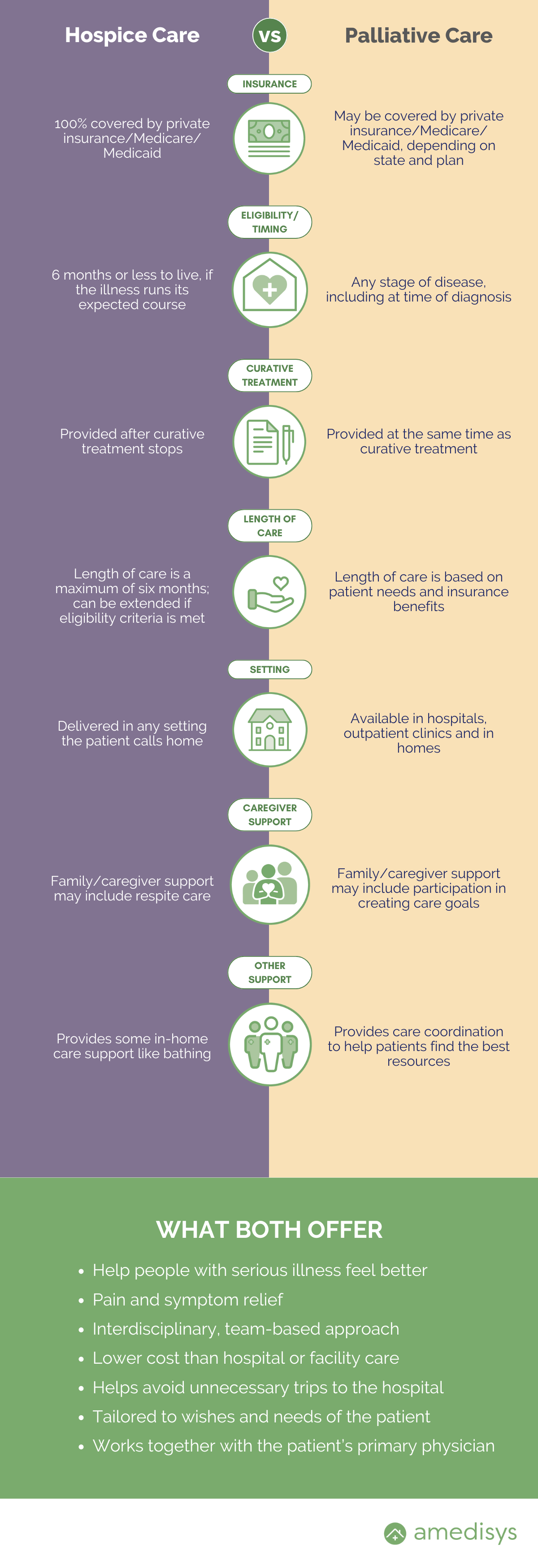
Hospice vs. Palliative Care Infographic
For a quick reference guide, see our infographic below or download it here.
Deb Gallaher, MSN, MBA, RN, NE-BC, CHPN, is a Senior Hospice Clinical Education Specialist for Amedisys. She has 10 years of experience in hospice and is passionate about sharing her insights on high-quality care.