[callout 1]
But what does an actual day in the life of a home health physical therapist look like? Meet Jeremy Lawson, physical therapist out of the Campbellsville, Kentucky home health care center. As soon as he wakes up at 7 a.m., he already has his mind on eating.
First, he cooks breakfast for himself and his wife, usually frying some eggs. Then he packs the food he’ll take with him for a day out on the road: typically, an apple for a mid-morning snack, a turkey sandwich for lunchtime and some chips or a protein bar to ward off a mid-afternoon slump.
No wonder Jeremy is so concerned about fueling his clinical adventures. Before the day is done, he’ll visit anywhere from six to eight patients. Each visit takes about 45 minutes, though a recent knee replacement patient required more like an hour and a quarter, with 20 minutes set aside just for an introductory education. And of course, he drives from one home to another to deliver his expertise.
Interested in becoming a home health physical therapist for Amedisys? Find open opportunities in your area!
By 8:15 a.m., Jeremy gets on the phone for a patient care conference call with his local office. They discuss new patient admissions, recent hospitalizations, potential discharges and other pending care transitions.
[action 1]
They also address how best to meet current staffing needs, convey relevant information about particular patients under care and synchronize schedules among clinicians. A recent call also touched on seasonal health issues – cold weather, for example, may spell flu, special difficulties with COPD and spills on icy sidewalks.
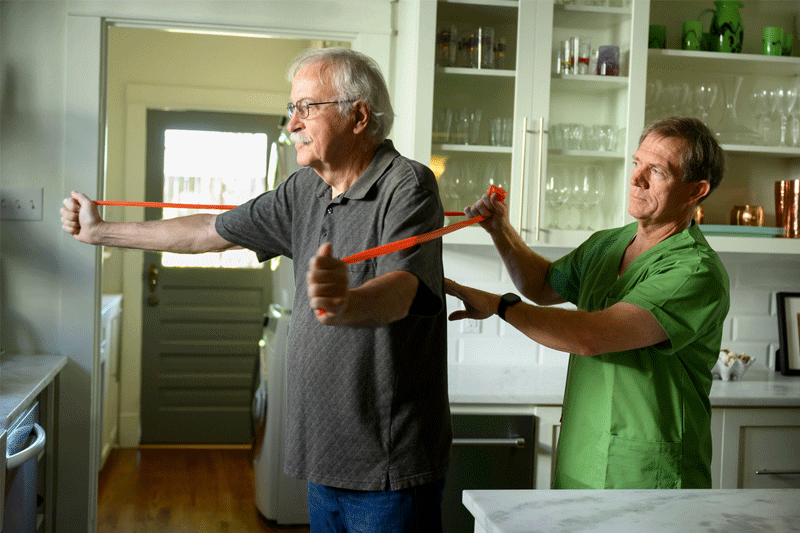
By 9 a.m. Jeremy arrives for his first patient visit. He’s currently caring for a patient recently hospitalized for flu who came home suffering from muscle atrophy, chronic low-back pain and generalized weakness, putting him at risk for falls and other issues. To start, Jeremy tested the patient to identify which movements might either ease or aggravate tightness or pain. Learning which motions felt comfortable and which hurt enabled him to establish an effective exercise regimen. He then designed a plan to build strength and improve balance and flexibility, including lumbar stretches.
Jeremy also sees patients for stroke, COPD and diabetes, among other conditions. He recently treated an amputee in need of adapting to a new leg prosthesis. The process entailed stretching that would link tissue with muscle and enhance flexibility.
Throughout his day, Jeremy documents each visit while he’s in the patient’s home, while the information is fresh in his mind—and he can involve the patient in their care. This also frees up his evening to focus on family and fitness, since he has already written out his notes for the day’s visits.
By 4 or 5 p.m. Jeremy heads home to do his daily workout. He logs 60 to 90 minutes, and usually gets in a two-mile run. He’ll also hoist dumbbells, focusing one day on biceps and triceps, the next day on chest and shoulders, and another day on legs and back.
“It would be hypocritical of me to tell patients to work out all day without doing my exercises, too,” the former high school and college soccer player admits. “As a physical therapist, you have to be an athlete and watch your body mechanics.”
At 6 or 7 p.m. Jeremy calls patients he’ll be visiting the next day. It’s mainly a heads-up to confirm his schedule and map out his route, but it’s also an opportunity to ask patients how they’re doing and find out if they just want to talk about anything. “Nothing is more critical to my daily schedule than these calls,” he says.
And so it goes as Jeremy Lawson simply does what physical therapists do. He quietly and tenderly ministers to his patients in their homes, whether they’ve sustained a stroke or spinal cord injury, undergone a hip replacement or are confronting injuries and other impairments. Week after week, he teases out movements that were all but unthinkable only moments earlier. Every inch is a milestone, a small step toward independence.
In those strenuous sessions, Jeremy helps train his patients to regain basic skills taken for granted since childhood but recently lost or compromised. Patients can learn to restore mobility and resume taking take care of themselves. They often can once again stand, walk, bathe, dress, swallow and eat independently.